Addressing disease hazards in the dental setting
Time spent at a medical office, where illness is expected, can create a fair amount of apprehension. One person’s persistent sneezing causes another to reach for an extra dollop of hand sanitizer. A patient’s wracking cough makes those in the vicinity think twice before taking a deep breath.
Visiting the dentist’s office doesn’t necessarily prompt that reaction, but the risk of contracting a serious infectious disease is just as real as catching a minor cough or cold. There are myriad factors dentists take into consideration in order to create a safe and sterile environment for patients, from the cleanliness of office surface areas to the water used for rinsing and the methods of instrument cleaning.
Safeguarding dental instruments
While in recent decades a handful of global pandemics have spread through air and contact — like tuberculosis, H1N1 and severe acute respiratory syndrome (SARS) — serious infectious diseases such as HIV, AIDs and hepatitis are actually simpler to prevent than airborne illnesses, says Dr. Raghunath Puttaiah, an associate professor at Texas A&M University Baylor College of Dentistry.
“Infections spread through saliva and blood are easier to control, because there are so many adequate precautions,” says Puttaiah, who teaches infection control and occupational safety at the dental school and trains dentists internationally on the subject.
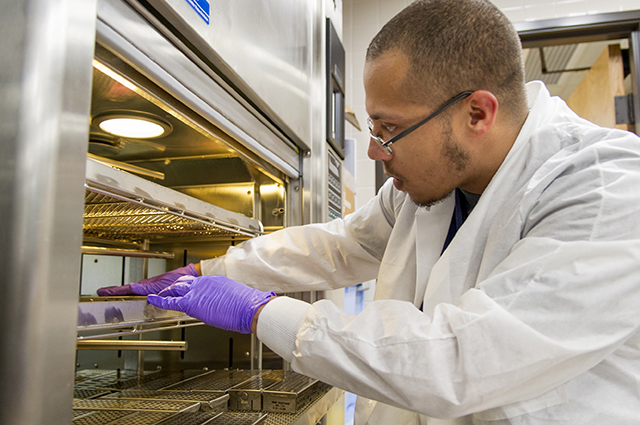
Chief among those measures at Texas A&M Baylor College of Dentistry is a centralized system for instrument sterilization. Because dental instruments come into direct contact with saliva and blood, they present the potential for conditions such as herpes, hepatitis and HIV. To mitigate this risk, instruments go through a stringent cleaning and steam heat sterilization process, which when used and monitored correctly, destroys all known bacteria.

After dental instruments are cleaned in washers, they are sealed into sterilization packs and placed into one of three large autoclaves, or pressurized chambers. Heat-sensitive tape on the packs indicates that the autoclave has reached the required temperature: 270 degrees.
In private practice, many dental offices use the same method, just on a smaller scale.
“Most dental practices do not have the volume of equipment that a school setting has; therefore, their needs are usually met through the use of a small autoclave such as a ‘Lisa,’” says Vickie Thompson, director of dispensing operations at the dental school. The college utilizes these smaller autoclaves — comparable in size to toaster ovens — in several of its dispensaries.
Monitoring water lines
Water goes hand in hand with a trip to the dental office. It is used to flush debris and polish from teeth during routine cleanings, and it acts as a coolant during lengthy procedures. But when water lines aren’t properly monitored and maintained, tiny microbes can form, leading to allergies or reactions in patients with compromised immune systems. Also at risk, Puttaiah says, are older patients and very young children.
Myra Spurgin is an infection control officer at the college and oversees water line maintenance and cleaning. Texas A&M Baylor College of Dentistry, like most dental schools, operates on a closed water system. Instead of running city water to each operatory, a water bottle is attached to every dental chair. Once filled, a preservative tablet is added, and water lines are cleaned only with products approved by the U.S. Food and Drug Administration and Environmental Protection Agency.
“You can regulate water lines better when you have a closed system,” Spurgin says. “Private practices may be hooked up directly to municipal water supplies, but they may only have three or four operatories.” Texas A&M Baylor College of Dentistry, by comparison, has 314 dental chairs.
Using protective equipment and common sense
Just as important for dentists, dental hygienists and assistants, Thompson says, is personal protective equipment, including gloves, a mask, and protective eyewear and apparel.
Avoiding common hazards in the dental environment begins with a shift in mindset, she says.
“Just because it’s not bloody doesn’t mean it’s not there,” Thompson says. “You have just as many infections in saliva and spray from your handpiece.”
Airborne diseases with the potential to spread at a rampant pace can be best prevented through basic tenants of infection control as well as common sense, says Puttaiah. Every dental practice is required to have a manual with occupational safety standards, which call for frequent hand washing and intermediate-level, hospital-grade disinfectants for cleaning equipment and work surfaces.
Don’t underestimate the importance of a phone call, he adds.
“We let the patients know that if they are not feeling well, it’s best not to come,” Puttaiah says. “If they have symptoms of not feeling good or feeling listless, we ask them to stay home. The same thing applies to staff.
“Constantly keep your ears open, eyes open and follow the fundamental principles of infection control.”
Puttaiah’s words mirror a unifying mindset in dental schools and dental practices nationwide: that infection control doesn’t just begin the moment the patient reclines in the dental chair. It’s an ongoing process of implementing, maintaining and refining with one priority in mind — the safety and comfort of patients.