Jump start

When someone goes into sudden cardiac arrest, time becomes critical. With each passing minute, the probability of survival decreases by 10 percent. After five minutes, permanent neurological damage is probable, and within 10 minutes, the episode is typically fatal. When you consider that response time to a 911 call can take up to 12 minutes, it’s no surprise that the only effective treatment — automated external defibrillators, which shock the heart back into a normal rhythm — is required by law in many public gathering places.
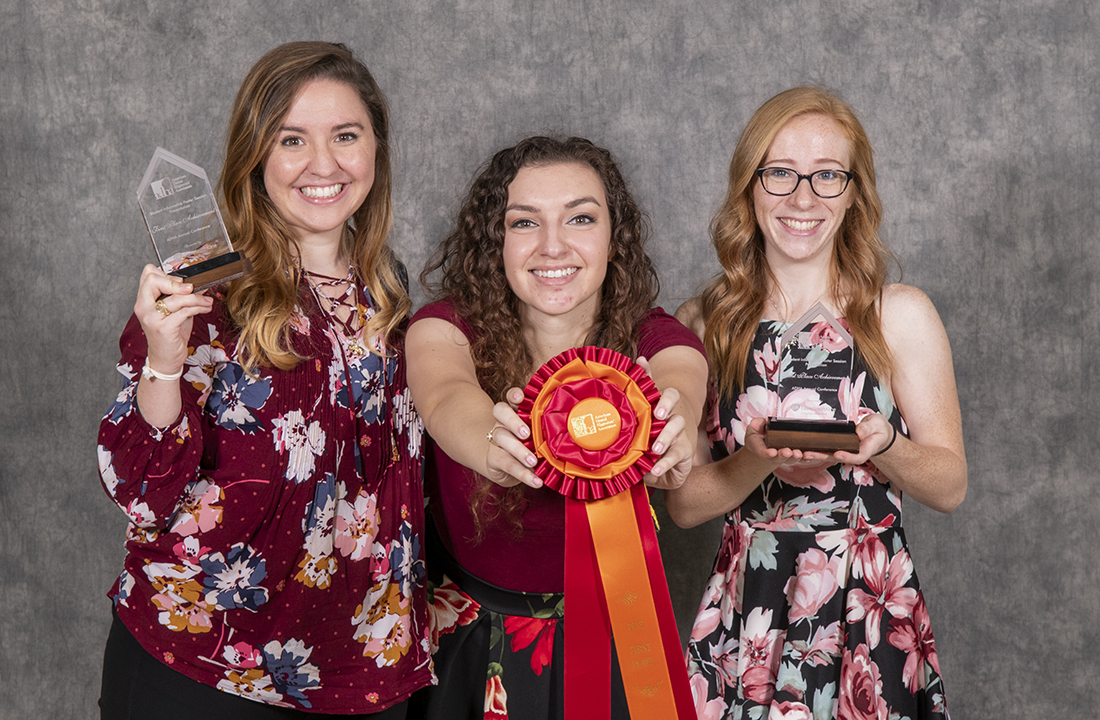
Last summer, then incoming second-year dental hygiene students Ashlyn Atwell, Briana Garza and Nina Matheney noticed an inconsistency between their licensure requirements and state law surrounding AEDs. Why were they required to have basic life-saving training with AED certification if Texas statutes didn’t require the life-saving device to be present in every dental office?
“Sudden cardiac arrest may manifest without warning, which is why the best prevention is being prepared.”
—Dr. Faizan Kabani
As part of their dental hygiene research course that fall, the students did some digging, and they discovered that while sudden cardiac arrest is one of the most common emergencies experienced in a dental office, the state only requires AEDs to be available in offices where low- to moderate-risk patients will undergo sedation or anesthesia. Even though AEDs are mandated in schools and nursing homes, this universal standard is not afforded to dental health care settings.
“It’s a very interesting topic with national implications, especially in regard to individual states’ dental practice acts,” says the group’s mentor Eric Fox, clinical assistant professor in Texas A&M College of Dentistry’s Caruth School of Dental Hygiene. “In my personal experience, I would say AEDs in the dental office are an exception, not the norm.”
The topic caught the attention of student and practicing dental hygienists alike, winning first place in the Student Informative Poster Presentation Competition at the American Dental Hygienists’ Association annual meeting in late June.
The accolades didn’t come without significant hard work, says Fox.
“Their biggest obstacle came at the beginning of their research, and that was finding appropriate research studies and legal cases for their literature review. In the end, they did find what they needed.”
Among the findings: While one of the biggest barriers to having an AED in the dental setting is cost — most range from $1,500 to $3,500 — the perceived lack of need and lax regulation both come in a close second. Patients most at risk in deregulated states such as Texas include those who are silently anxious, have undiagnosed heart problems or experience severe allergic reactions to dental materials.
The compelling statistics, combined with a polished presentation, contributed to the win.
Now the three recent graduates are pursuing publication in Dimensions of Dental Hygiene for early 2019, says Dr. Faizan Kabani, assistant professor, who oversees dental hygiene student research.
“This topic should be of significant concern to all dental professionals,” says Kabani. “There have been multiple documented legal cases that our graduates also cite where dental providers’ licensures were suspended — some for a decade — for failure to provide emergency management by not having access to emergency equipment, one of which included a defibrillator.
“Sudden cardiac arrest may manifest without warning, which is why the best prevention is being prepared. Imagine how much we can contribute to improving our patients’ quality of life if we are collectively prepared with AEDs in our dental offices.”