Not enough dentists?

More than 47 million Americans live in dental underserved areas. Within these areas, the amount of dental needs that are actually met hovers right around 40 percent, according to a Health Resources and Services Administration report. Based on this same report, more than 7,300 more dentists would be needed to fill all the dental needs in the U.S.
In a recent article published in the Journal of Public Health Dentistry, Texas A&M College of Dentistry researchers dive deep into several national databases to shed more light on what is actually occurring in these dental shortage areas. How do income and education levels, population density, and location fit into this picture? And most importantly, what can be done to fix the problem when current public programs and market forces have failed to do so?
What they did
In July 2014, Dr. Andreea Voinea-Griffin had barely unpacked her office after joining the College of Dentistry faculty when she and Dr. Eric Solomon forged a collaboration. Solomon, research professor and executive director of institutional research, analyzed HRSA-designated dental underserved areas, comparing their populations to those in geographic areas not designated as underserved, and pored over the characteristics of dental practices located in each of these areas. He looked at details such as sales volume, number of employees and practice square footage. This served to pinpoint the relationship between distribution of dental practices, characteristics of those practices and the populations most likely to experience shortages. Voinea-Griffin, research assistant professor, studied the impact of public health policy on these particular areas.
“What Andreea brings to the table is the policy part,” Solomon says. “She looks and says, ‘These are the kinds of things that have been done before, and these are the kinds of things that can be done in the future.’”
What they found
It didn’t take long for a pattern to emerge, which revealed that dental underserved areas are more likely to have:
- residents with lower income and education levels;
- higher levels of underrepresented populations;
- lower population densities; and
- geographic, financial and educational barriers to care.
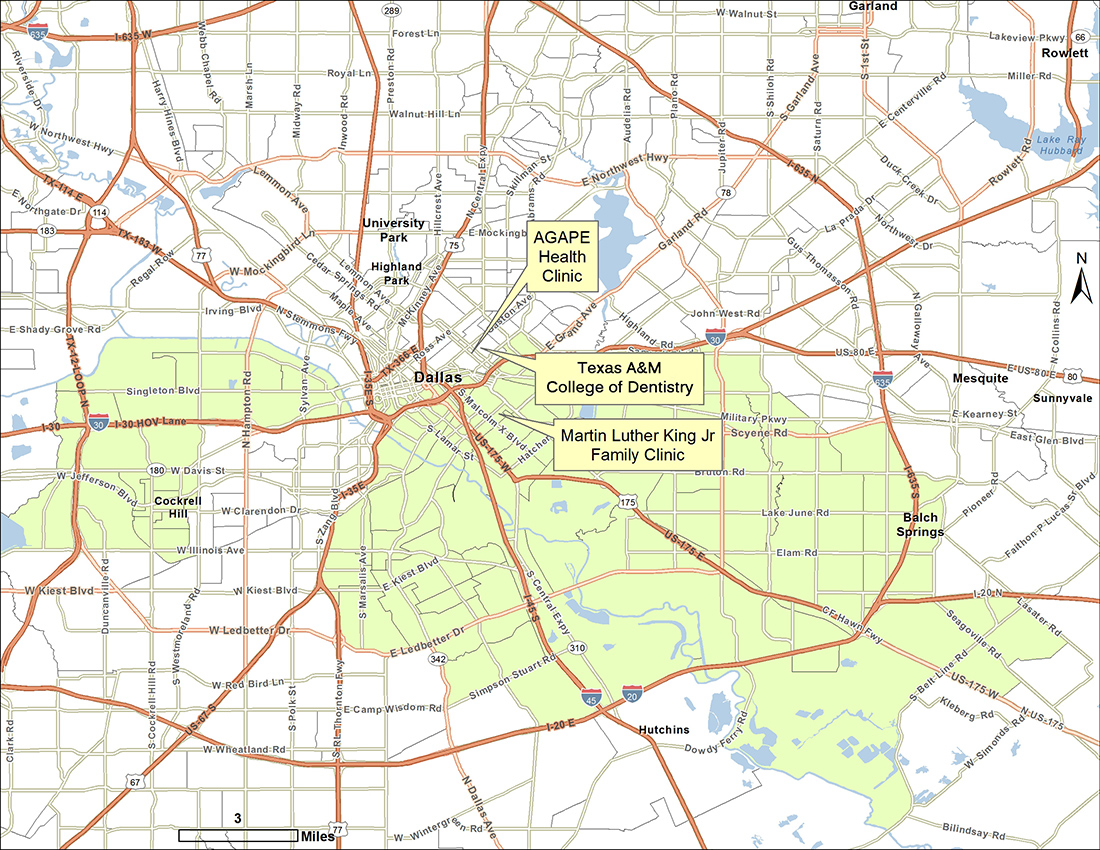
Two such areas are in the college’s backyard, to the east and west. Because the government divides populous, urban areas by census tracts, instead of zip code, the characteristics of these areas accounts for the underserved status.
“Our findings pinpoint the actual issue,” Voinea-Griffin says. “It builds the argument toward a possible solution, because in this case you would expect that dentists don’t go to areas of low socioeconomic status because there is not money to be made there. You would expect that. It’s common sense. When you step back, you think, ‘What is the solution?’ You can’t really make anyone go there. Market forces won’t fix it. Because if they did, it would have happened by now.
“It’s pretty widespread across the country, so waiting and expecting things to solve themselves is not really a solution; it’s actually more of a confirmation for policymakers that this can’t fix itself.”
What can be done
The study explored the underlying concern that simply increasing the number of dental school graduates nationwide may not address existing dental shortages. If new dentists choose to practice in other locales, needs in underserved areas will remain unmet.
Accordingly, one solution could involve incentivizing graduates to underserved areas through student loan repayment programs. Such a solution would require the addition of public health clinics to these areas. Other possibilities, says Voinea-Griffin, could involve regularly scheduled mobile dental units that bring care to patients, helping mitigate geographic barriers. As Medicaid expands in several states to include increased adult dental coverage, financial concerns may also be addressed.
By comparison, large-scale dental events, such as Operation Lone Star, in which college students and faculty provide free care to hundreds of patients in South Texas for a week each summer, may be beneficial, but they don’t correct the bigger issue.
“One day or one week every six months won’t solve a problem,” says Voinea-Griffin. “You need regular care and a regular schedule.”
“The goal is to have a dental home,” Solomon adds.
Loving County, Texas, population: 112
 Geographic barriers to care require special consideration in states such as ours, with its vast, open spaces. Nearly 4 million Texans live in dental underserved areas, but with giant swaths of land often dotted with sparse populations, the numbers take on a different tone. Take, for instance, the roughly 23,000 square mile, eight-county spread in West Texas with only 1.36 residents per square mile, served by just five dentists.
Geographic barriers to care require special consideration in states such as ours, with its vast, open spaces. Nearly 4 million Texans live in dental underserved areas, but with giant swaths of land often dotted with sparse populations, the numbers take on a different tone. Take, for instance, the roughly 23,000 square mile, eight-county spread in West Texas with only 1.36 residents per square mile, served by just five dentists.
“Market forces can’t solve the problem, but if you are going to designate an area as underserved, there should be some consideration about whether this is a feasible area to locate a practice,” says Solomon. “There are a lot of places that don’t have the population threshold to sustain a practice.
“These counties out west are big. It’s not only money. It’s how you get people to care.”