Progress notes
It’s a new era in treating head and neck cancer.
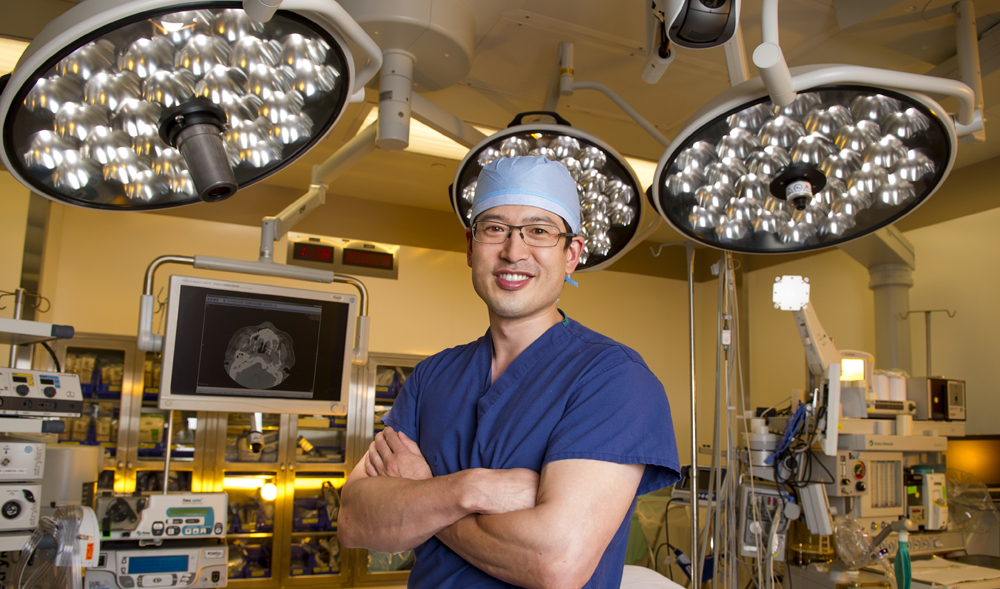
Meet Dr. David Kang, assistant professor in oral and maxillofacial surgery and the department’s first head and neck oncologic and microvascular reconstructive surgeon. The description is complex, but the meaning isn’t lost on patients with oral cancer facing the reality of surgery.
After receiving his dental degree from Columbia University and finishing medical school and his residency at UT Southwestern Medical Center and Parkland Memorial Hospital, Kang felt so drawn to the subspecialty that he spent an additional year of training completing a fellowship in head and neck oncologic surgery at the University of Michigan. He has returned to Dallas with the in-depth training he needs to not only remove cancerous head and neck tumors but also reconstruct the entire surgical area — providing a critical step in a patient’s return to normalcy following a life-altering diagnosis and treatment.
Most of the time you can find Kang at Baylor University Medical Center’s Truett Hospital, prepping for surgery in his scrubs, surgical mask and cowboy boots, but we caught up with him one Friday afternoon to learn more about the multidisciplinary approach to treating head and neck cancer, the surprising source of tissue used to reconstruct the oral cavity and — on a personal note — the best part of being back in Dallas.
NewsStand: How do you anticipate coordinating a multidisciplinary approach to caring for cancer patients with the various medical oncology specialists involved in their treatment? Who is most likely to refer patients to you for surgical care?
Kang: Head and neck cancer is managed by a large team that includes radiation oncologists, medical oncologists, oral pathologists, surgical pathologists, speech, physical and occupational therapists, as well as home health and hospice. Our patients are frequently presented to the Head and Neck Tumor Board, which meets at the Baylor Charles A. Sammons Cancer Center the second and fourth Tuesday of the month. At this meeting we discuss treatment options including surgery, radiation therapy and chemotherapy.
I expect most of my referrals to come from oral and maxillofacial surgeons and dentists in North Texas, since oral cancer patients are typically found by vigilant dentists who will notice a suspicious lesion and then refer the patient to an OMS specialist who biopsies the lesion. Depending on the results, these patients will then be referred to a surgeon who specializes in head and neck oncologic surgery. Several different specialties treat head and neck cancer, and these include oral and maxillofacial surgeons, otolaryngologists and general surgeons.
NewsStand: Many of the patients you treat deal with the reality of radiation — a treatment that, while often effective at combating cancer, is notorious for wreaking havoc on the environment in the mouth. What special steps must you take to ensure that the patient’s reconstruction holds up to the radiation that may occur post-surgery?
Kang: In the past, there was significant morbidity and decreased quality of life associated with oncologic resections resulting in loss of facial aesthetics, speech and ability to eat, sometimes leading to a hermetic lifestyle. With the advancement of microvascular reconstructive surgery, we can now take composite free tissue — skin, fascia, muscle, nerve, bone — to reconstruct any maxillofacial defect regardless of size and return form and function to the patient. Free tissue transfer — or free flap — has become the gold standard in reconstruction of the difficult three-dimensional aspect of the oral cavity.
The reason that free tissue transfer can withstand radiation therapy is that the artery and vein going to the flap are dissected out with the necessary skin, muscle and bone tissues and transplanted from another part of the body to the face, such as the fibula osteocutaneous free flap harvested from the leg. These vessels are then sutured to recipient vessels in the neck under our surgical microscopic, and once the vascular clamps are released, the flap and all the tissues brought with it are immediately revascularized. This gives immediate blood flow to the tissues and rapid healing of the surgical site, which allows the initiation of radiation therapy within four to six weeks.
NewsStand: Tell me about some instances in which reconstruction is not an option. In those situations how closely must you work with the college’s Center for Maxillofacial Prosthodontics to help restore the patient’s appearance and sense of normalcy?
Kang: Reconstruction is always an option, but it may not be the best choice for the patient. Reconstruction with free tissue transfer requires longer operating room time, a longer hospitalization and frequently a tracheostomy. The need for free tissue transfer is weighed against the patient’s medical status and their physiological age rather than chronological age.
We will often opt for placement of an obturator, which is very similar to a denture and closes off the defect as well as restores facial contour. Sometimes, reconstruction with free tissue transfer requires multiple surgeries and revisions, and the results may not look as good as a prosthetic, such as with a total rhinectomy. In the Department of Oral and Maxillofacial Surgery’s Center for Maxillofacial Prosthodontics, we have anaplastologist Suzi Verma, who can create beautiful reconstructions for our patients including noses, ears, eyes and portions of the face.
NewsStand: What’s the best part of being back in Dallas?
Kang: The weather and food are fantastic. The food culture is getting better every day, with delicious restaurants that seem to open every other week, excellent shopping opportunities and professional sports for every season. Dallas is a cultural hub for this region of the country, and we feel lucky to be part of this growing city.
—Jenny Fuentes