Regenerative medicine in dentistry: Making strides toward a 'bio-tooth'
NIH funding begins for TAMBCD researchers to unlock mysteries of tooth root formation
When it comes to regenerative medicine within dentistry, studies aimed toward whole tooth regeneration stand to revolutionize the future of dental treatment. There’s just one problem: In order to regenerate an entire tooth, researchers must first learn how to regenerate the tooth crown, the visible part of the tooth, and the tooth root, the portion under the gum line that is buried in bone and anchors the tooth in position.
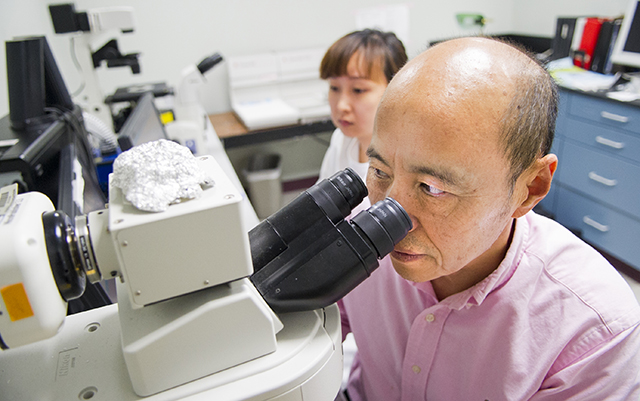
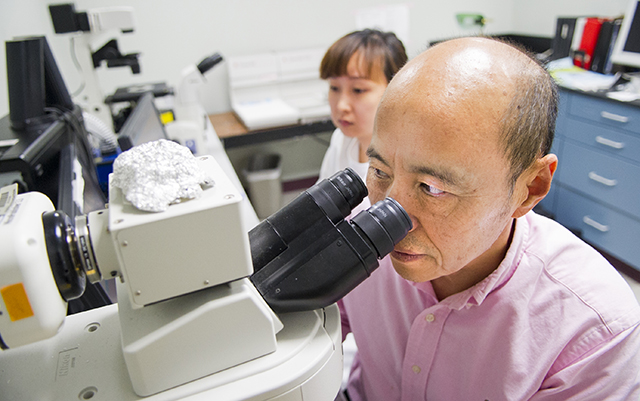
“With tooth regeneration, the problem is not in the crown, it’s in the root,” says Dr. Jerry Feng, professor of biomedical sciences at Texas A&M University Baylor College of Dentistry. “You can easily make a crown, but you can’t easily make a root.”
That’s because, contrary to prior belief, formation of the tooth root, composed of dentin, is different than in the crown, which forms prior to the root and is composed of dentin and enamel.
“The biology is more complex than what we used to believe,” says Feng.
In July, funding will begin on a $1.8 million grant from the National Institutes of Health – National Institute of Dental and Craniofacial Research that will allow Feng and TAMBCD researchers to further study the mechanisms involved in tooth root formation, which until now has been infrequently studied and not well understood.
“This has applications not only in science, in filling that knowledge gap, but also for future regeneration of the whole tooth,” says Feng. While a “bio-tooth” could provide an alternative to dental implants and restorations for problems ranging from dental trauma to periodontal disease, Feng explains that these potential uses won’t occur anytime soon.
“To regenerate the whole tooth, we have a long way to go — years, if not decades,” says Feng.
For this project, TAMBCD researchers will utilize transgenic and conditional knockout mouse models to investigate the role of osterix, a gene vital in skeletal formation but still a mystery in terms of its function in tooth biology. Preliminary studies in mouse models have already shown that while deletion of osterix has no impact on tooth crown or even the pulp chamber, which houses the tooth’s nerves, blood vessels and connective tissues, lack of osterix causes the tooth root to become stunted, thin and even fracture, signaling the need for its presence in tooth root formation.
In addition to osterix, the research will include a closer look at other factors impacting tooth root formation. With help from Dr. Stephen E. Harris, a professor in periodontics at the School of Dentistry at University of Texas Health Science Center San Antonio, they’ll compare the expression pattern of every gene in the tooth root versus the tooth crown through RNA- and next-generation DNA sequencing.
“One of the major causes of tooth loss is related to changes in tooth root biology,” says Harris, who has secondary appointments in the San Antonio dental school’s Department of Cellular & Structural Biology and Biomedical Engineering Program. “This research will discover new pathways and genes and open up new targets for regenerative medicine in the dental field.”